Affecting more than 6 million Americans, chronic plaque psoriasis manifests as patches of red, scaly skin most frequently on the scalp, elbows and knees.
Eczema / Psoriasis News From Medical News Today

Tag Archives: Chronic
Chronic Fatigue, histamine & mast cells
 Chalk up another one to a dysfunctional immune system – Chronic Fatigue Syndrome (CFS). Researchers recently proved (for the first time), that the condition is not psychosomatic (yeah, thanks for calling us hypochondriacs all these years). This wasn’t news to some: according to NHS funded researcher Dr. Theoharides, CFS is one of many mast cell linked conditions that he has known to be linked for years. It wasn’t so long ago that narcolepsy was pegged to an imbalance of brain histamine levels.
Chalk up another one to a dysfunctional immune system – Chronic Fatigue Syndrome (CFS). Researchers recently proved (for the first time), that the condition is not psychosomatic (yeah, thanks for calling us hypochondriacs all these years). This wasn’t news to some: according to NHS funded researcher Dr. Theoharides, CFS is one of many mast cell linked conditions that he has known to be linked for years. It wasn’t so long ago that narcolepsy was pegged to an imbalance of brain histamine levels.
Scientists in Australia have found that immune cell receptor abnormalities are behind CFS debilitating symptoms. So basically a receptor defect, which is really a problem because there are many cells and so many receptors to mess with, can’t transfer calcium from the cell to the outside. The discovery of abnormal calcium cells coincides with where CFS pain usually happens, in the brain, spine, pancreas and stomach.
To date there’s still no cure for CFS. Doctors and researchers have been telling folks it’s all in their head and that all they need is more exercise (yes, I’m referring to the PACE trial debacle). The researchers say they believe that it affects from 1%-2% of the population (presumably Australia they mean?).
According to Dr. Theoharides, director of Immuno pharmacology and Drug Discovery at Tufts, CFS is a complex disease involving the nervous, hormonal and immune systems with symptoms that include fatigue, sleep disturbances, malaise, muscle aches, migraines, gastrointestinal complaints, and cognitive problems. Viruses and inflammatory cytokines (like those in mast cells which contain histamine) play a role. He says that the stress hormone CRH (corticotropin-releasing hormone) activates brain mast cells (which contain histamine and other inflammatory mediators), and that this causes blood-brain-barrier disruption. His research shows that there’s a relationship between the mitochondria, calcium and mast cell activation.
As someone who has literally fallen asleep on a plate of food, I can attest to the narcolepsy-histamine link. It all depended on how long it would take me to eat. If I had a short meal, I might make it to the sofa before falling into my food coma, but a long one meant face-in-food for dessert. The weird thing was I wasn’t actually asleep.
My eyes were forced closed, all movement would have to cease, and I’d be aware of the world around me, but incapable of interacting with it. The experience was more like something out of a nightmare where you’re paralysed but still able to be hurt. It’s apparently called syncope.
I’d lie there in a weak panic, feeling my heart beat slowly ebb away, as I begged my thoughts to magically reconnect with my voice to tell people, hey, I’m actually awake! Don’t be fooled, I’m not asleep. But no matter how hard I tried to convey this to people, they were all convinced I was dreaming it all up.
Whether it was a histamine-narcolepsy link, or a mast cell-CFS one, I ended up spending about a year mostly in or on bed, and desperately trying to make people understand that my inability to climb a flight of stairs at times isn’t a lack of cardio fitness (mine could always be better but it’s still good) but rather a result of my mast cells having a temporary bout of madness.
Interestingly, Harvard neuroscientist Dr. Michael Van ElZakker has a hypothesis he’s working to prove, that an infection of the vagus nerve, which connects the brain to the stomach, can cause a prolonged “sickness response”. This human response to illness involves extreme fatigue, probably to force us to rest up and isolate us from other humans to not spread the virus. He believes that in some cases the vagus nerve, which is responsible for signaling the need for this response, remains on high alert, which keeps the body stuck in this more.
You can read my interview with Dr. Van ElZakker here.
A review of fourteen separate dietary and supplement interventions were published in the Journal of Human Nutrition and Dietetics, but found that most studies showed no particular measurable benefit of them. Improvements in fatigue were found in response to NADH and Coenzyme Q10, probiotics and high polyphenol rich cacao.
For me personally, because my fatigue was a result of my mast cell issues, stabilizing them with Dr. Theoharides’ quercetin Neuroprotek supplement and a great diet really helped. But we all have different root causes and severity of symptoms.
Click here if you’d like to learn how I did it.
It’s finally here! Man Food – a high nutrient antihistamine and anti-inflammatory ingredient filled book geared towards guys, women who love to work out, yoga like they mean it, or just load up on healing nutrients. Features my personal shopping list of antihistamine and anti-inflammatory foods.
The Anti-cookbook and all liquid Anti-Detox Book, don’t treat any conditions, but feature a plethora of the high nutrient antihistamine and anti-inflammatory ingredients that have been instrumental in helping me feed myself on a limited diet. The Anti-cookbook features a four page list of antihistamine and anti-inflammatory foods and comes in regular and Paleo.
The Low Oxalate Cookbook features antihistamine and anti-inflammatory rich recipes.
Don’t miss the Low Histamine Beauty Survival Guide for non-toxic beauty tips, the skinny on histamine releasing (mast cell degranulating) beauty ingredients, antihistamine and anti-inflammatory beauty alternatives and the top brands natural brands I’ve found.
Take a peek at my other low histamine and antihistamine cookbooks for more high nutrient recipes
—–REFERENCES—-
Theoharides, Theoharis C. “Brain mast cells and Chronic Fatigue Syndrome.” Grantome. NIH, 01 July 2012. Web. 24 Mar. 2017.
Appold, Karen. “UCLA Researchers Find Clue to Narcolepsy’s Cause.” Sleep Review. N.p., n.d. Web. 24 Mar. 2017.
Campagnolo, N., S. Johnston, A. Collatz, D. Staines, and S. Marshall-Gradisnik. “Dietary and nutrition interventions for the therapeutic treatment of chronic fatigue syndrome/myalgic encephalomyelitis: a systematic review.” Journal of Human Nutrition and Dietetics (2017): n. pag. Web.
Cooper, Luke. “Queensland Scientists Make Chronic Fatigue Syndrome Research Breakthrough.” Huffington Post Australia. The Huffington Post, 21 Feb. 2017. Web. 24 Mar. 2017.
Rehmeyer, Julie. “How bad science misled chronic fatigue syndrome patients.” STAT. STAT, 29 Dec. 2016. Web. 24 Mar. 2017.
Back in business: treatment options for lower and chronic back pain
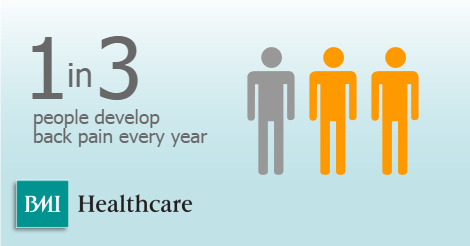
While back pain can be debilitating and distressing, there are a number of treatment options available. As the largest private hospital group in the UK, BMI Healthcare are used to providing a range of options and treatments for back pain, read there article below and find out what you can do.
Intro
Each year, 1 in 3 people develop back pain(1). In most instances, people experience moderate pain in the lower back which can be managed with over-the-counter painkillers. Lower back pain is extremely common, affecting about 4 in 5 people at some point in their life, usually between the ages of 30 and 60. It can last days, weeks or even months. When pain continues for over three months, it becomes known as chronic back pain.
Back pain – especially chronic back pain – can affect people’s mood, sleep, work and quality of life. While it’s often difficult to identify the exact cause of back pain, it’s usually related to strained muscles, tendons or ligaments, or other structural damage.
Surgical and non-surgical treatment
The use of surgery to treat back pain is quite rare; there are a number of non-surgical treatment options available, and spinal surgery will usually only be offered as a last resort if these treatments prove ineffective.
Indeed, unless you have a condition that specifically requires surgical intervention, doctors are likely to recommend painkillers, psychological therapies, exercise and physiotherapy, acupuncture or pain management before they opt for surgery. The most common conditions corrected by spinal surgery include prolapsed discs, which cause nerve symptoms in the neck and back, along with chronic neck and back pain.
Types of spinal surgery
However, if surgery is required, there are several types of intervention to consider. Some interventions are intended to relieve back pain caused by wear and tear, while others target limb pain – for example, sciatica in the leg caused by nerve pressure in the spine.
Your GP will help to determine whether or not you require back surgery. If a disc in your back has become damaged and is putting pressure on the surrounding nerves – sometimes referred to as ‘a slipped disc’ – you could be offered a discectomy. This procedure involves removing the whole or part of one of the discs between your vertebrae.
For a condition known as spinal stenosis, which causes the space inside your spine to narrow, you may undergo a laminectomy. This involves removing a small part of the bone called the lamina at the back of your vertebra.
Spinal fusion, meanwhile, is a procedure to join two or more vertebrae together using bone grafts, rods and screws in order to strengthen and stabilise the spine and prevent pain caused by movement. A spinal fusion may be recommended if you have a condition such as spondylolisthesis, whereby one of your vertebrae slips out of place, or if you suffer from severe degenerative disc disease.
Damage to vertebrae can also be repaired using a procedure known as vertebroplasty, which involves injecting a bone-cement into the vertebra. This procedure is often used to treat compression fractures caused by trauma or osteoporosis(2).
Be prepared
The back is a complex structure made up of bones, muscles, ligaments, tendons, joints and nerves. The spine supports the back and is made up of 24 separate vertebrae; it also encases the spinal cord, which carries nerves from the brain to the rest of the body.
Surgical intervention in such a crucial part of the body is no small undertaking and not a decision that should be taken lightly. If it’s recommended that spinal surgery is the best course of action available to you, you must make all necessary preparations in advance of your operation.
While most people can walk after back surgery, in the first days after an operation simple, everyday tasks such as lifting, driving, washing, cleaning or dressing may be painful and problematic. You may want to ask a friend or family member to help you during this time. You’ll certainly need someone to pick you up from the hospital.
If you smoke, you may be asked to stop before your operation, as smoking increases the risk of chest and wound infection, which hampers the recovery process. In the hours before the operation, you’ll most likely be asked not to eat or drink as most back surgery involves a general anaesthetic. In addition, during your time in hospital you’ll probably be asked to wear compression stockings to help prevent blood clots forming in your legs.
A personal choice
Ultimately, the final decision to proceed with spinal surgery lies with you and you alone. Your doctor and surgeon will discuss the options with you, but if you decide not to go through with surgery then they will respect your wishes.
Furthermore, pain is personal and subjective, and the way in which it is treated is down to the preferences of the individual involved. Back pain can become debilitating and severely impact your quality of life; some people opt for surgery, while others choose to manage their pain through physiotherapy and alternative therapies, such as acupuncture.
Whatever route you select, it’s vital to ensure your treatment pathways not only give you a chance to live a life free of pain and discomfort, but that they are appropriate for you and that you are happy with the choices you make.
To find out more and discuss your options with BMI Healthcare please get in touch and make an enquiry.
(1) http://www.bupa.co.uk/health-information/directory/b/back-pain
(2) http://www.bupa.co.uk/health-information/directory/b/back-surgery
Key to chronic eczema itch may lie in special ion channel
Recently scientists reported the discovery of an “itch molecule” (Nppb) responsible for conveying the itch signal across the synapse from sensory neurons in the skin to neurons in the dorsal horn of the spinal cord.
The media made a great deal of this study, which laid out a substantial model for how we feel itch.
Something I hadn’t noticed, though, was that the Science study considered only a subset of neurons involved in sensing itch—those that are activated by histamine. These neurons, at the itch-sensing end, have a type of ion channel called “TRPV1” that detects histamine and other substances, or “pruritogens,” that induce itch.
An ion channel is a kind of gate that opens when a key–such as a histamine molecule–binds to it. The open gate lets in sodium or potassium ions. When this happens to ion channels in a neuron, the neuron sends an electrical pulse down its length, transmitting information, such as a sensation of itch.
But there are other triggers for itch besides histamine. “Histamine-independent” itch is particularly important in the chronic itch experienced by eczema patients. (And that’s why antihistamines don’t do us any good.)
Histamine-independent itch is transmitted by neurons that possess TRPA1 ion channels. A new study, published in the Journal of Neuroscience, shows that mice only feel chronic itch if they have neurons expressing TRPA1 channels. Strikingly, the scientists show that knocking out TRPV1 channels (the histamine-dependent kind) does not affect the ability of mice to feel chronic itch.
As a model of chronic itch, the researchers shaved the cheeks of lab mice and exposed the skin to drying chemicals over a period of a few days. The mice scratched their cheeks and developed classic signs of dry, itchy skin–unless their TRPA1 channels had either been genetically deleted or inhibited by a drug,in which cases they hardly scratched at all.
The researchers were also interested in whether the itch-scratch cycle affected the sensation of itch. If you don’t scratch an itch, does it get better or worse? The answer appears to be that if you (or, by proxy, a lab mouse) have an itch on your back that you can only scratch by rubbing it against the wall, it may torment you, but when measured by objective standards, skin that you don’t scratch ends up in better shape.
We can draw two practical conclusions from this work, which was led by Diana Bautista at UC Berkeley: that blocking TRPA1 channels with a drug in cream or ointment form could be a potential solution to the chronic itch of eczema; and that it really does appear that if you can break the itch-scratch cycle, your skin will be better off.
Now, we all know how difficult it is to stop scratching. It’s not as easy as saying that you’ll stop. But this type of research certainly highlights the positive feedback of habit-reversal, which uses psychiatric techniques to reduce habitual scratching. Scratch less…and you’ll feel less itchy.
I do have one question: does the molecule Nppb, reported in the Science paper two weeks ago, transmit chronic itch signals as well as histamine-induced itch? If so, it is still a valuable target for further research into eczema therapies.
End Eczema
Natural Treatments for Chronic Eczema
Chronic eczema is one of the more unpleasant conditions which you can suffer from. It’s not harmful in general, but that’s not the problem. It’s very unpleasant visually, and can reduce your self-esteem dramatically.
You have to come to terms with the fact that there is still no cure for this disease through the use of medicines, all you can do is to keep it under control. Quite a lot of people who have used medications and drugs for their eczema have started to now use more effective natural methods, they have gone on to say these natural methods have worked better for them.
Begin by looking at any potential eczema allergies. They are the core reason for chronic eczema’s reappearance, as it is highly sensitive to any allergic reactions your body has. It’s not always easy to try and work out what is the cause behind your condition, but once you can become aware of this, your life will become a whole lot easier.
Some common places to start looking at when trying to determine your allergies, are soy, eggs, cow’s milk, and such products. Salt water and oatmeal are really good for helping to control your eczema plus they are completely natrural treatments. Using oatmeal and sea water have been proved to be very effective. Oatmeal is useful for relieving inflamed areas of the skin, and it’s a commonly used ingredient in some lotions. If you have a itchy rash rub some oatmeal paste on, it will help to calm it down. When you take a bath add oatmeal to the water, this is a good natural method for controlling your eczema.
Sea water is useful in the same way. Sea salt is an antiseptic, and you can mix it with the water you bathe in to achieve the desired effects. As sea-water has shown to be pretty effective, it is now used as a of treatment for controlling your eczema. Give the sea salt a go, it can definitely help your eczema.
Light treatment is another not so popular method, but a lot of people have reported it helping them greatly. Phototherapy is something you might consider, especially if you notice your eczema improves whilst your out in the sun.
Coming to terms with eczema can be very difficult. Even though it can get really tough, you have to carry on fighting. You must remember that medications will only help your eczema for so long. More and more sufferers are starting to use more natural treatments for chronic eczema, and these are proving to be extremely useful for relieving the condition, and in some cases eradicating it altogether.
Natural treatments for chronic eczema are being used by many people to significantly reduce their condition. Not only are these treatments effective, they also avoid the pitfalls associated with the side effects from medications. As a sufferer from chronic eczema, it is something that you should be looking at.
Risk For Basal Cell Carcinoma Can Be Chronic
AppId is over the quota AppId is over the quota Main Category: Melanoma / Skin Cancer
Also Included In: Dermatology;??Eczema / Psoriasis
Article Date: 27 Jul 2012 – 1:00 PST Current ratings for:
Risk For Basal Cell Carcinoma Can Be Chronic 

In the powerful sunlight of July, newly published results from a large study of people at high risk for basal cell carcinoma support the emerging view of the nation’s most common cancer as a chronic ailment that often repeatedly afflicts older people but for which the seeds may be planted in youth. The research also found a new association with eczema.
“Basal cell carcinoma is a chronic disease once people have had multiple instances of it, because they are always at risk of getting more,” said Dr. Martin Weinstock, http://www.eczemablog.net/professor of dermatology in the Warren Alpert Medical School of Brown University, who practices at the Providence Veterans Affairs Medical Center. “It’s not something at the moment we can cure. It’s something that we need to monitor continually so that when these cancers crop up we can minimize the damage.”
Dermatologists hold out hope for a medication that will help prevent recurrences of BCC. To test one such medicine, Weinstock chaired the six-site, six-year VA Topical Tretinoin Chemoprevential Trial, which last year found that the skin medication failed to prevent further instances of BCC in high-risk patients.
Weinstock is the corresponding author of the new study, published online July 19 in the Journal of Investigative Dermatology, which presents an analysis of the risk predictors of BCC recurrence found among the trial’s population of 1,131 people, all of whom were veterans, 97 percent of whom were men, and whose median age was 72. On average, a participant had more than three episodes of BCC or squamous cell carcinoma before entering the study.
History, eczema, and early exposur
Overall, 44 percent of study participants developed new BCCs during the study period. The biggest predictor of another bout with BCC after three to four years of follow-up was a prior history of them. The 129 participants who had more than five BCCs in the five years before the study had a hazard rate ratio that was nearly four times as high as that of the 204 people who had none or one and more than twice as high that of the 200 people who had three.
Eczema was another predictor of BCC recurrence in the study’s high-risk group. Participants who acknowledged a family history of the skin condition had a hazard rate ratio 1.54 times higher than people who did not, after statistical adjustments.
“We don’t know why this is,” Weinstock said. “The connection with eczema is something that’s new, that needs to be further explored.”
Age was another predictor, and not just in providing further confirmation that the risk people face increases with age. The study also showed that particularly intense sun exposure before the age of 30 was a strong a predictor of BCC occurrence among the high-risk study population, even though for most of them their 30s were decades ago.
“We talk about sun protection, which is important, but that’s something for basal cell that’s most important in your youth,” Weinstock said. “While we don’t exonerate UV exposure in one’s 40s, 50s, and 60s, it was particularly UV exposure before the age of 30 that was most closely related to BCC in our study.”
Awaiting a new trial
If limiting UV exposure is most crucial before the age of 30, what can doctors do for older people who may be headed for multiple bouts with BCC?
“Right now we have this wait and cut approach,” he said. “We know these people are at high risk and we know that most of them are going to get more.”
A better solution comes back to finding and testing preventive medication. Tretinoin didn’t work, but Weinstock said he and his colleagues are testing another called 5-Fluorouracil. He said he is optimistic but has not yet seen the data from a trial that began about three years ago.
Article adapted by Medical News Today from original press release. Click ‘references’ tab above for source.Visit our melanoma / skin cancer section for the latest news on this subject. Robert Dyer of the Providence VA Medical Center and Brown University was the study’s lead author. In addition to Dyer and Weinstock, other authors on the paper are Tobias Cohen, Amilcar Rizzo, Stephen Brigham and the VATTC Trial Group.
The U.S. Department of Veterans Affairs Co-operative Studies Program funded the research.
Brown University Please use one of the following formats to cite this article in your essay, paper or report:
MLA
7 Apr. 2013.
Please note: If no author information is provided, the source is cited instead.
posted by Dr. J on 28 Jul 2012 at 7:22 am
Topical 5-FU is an excellent treatment for superficial basal cell or actinic keratosis! It is widely underutilized! If your dermatologist only thinks to cut is to cure, you would be wise to get other opinions. If effective, it heals with no scaring!
| post followup | alert a moderator |
‘Risk For Basal Cell Carcinoma Can Be Chronic’
Please note that we publish your name, but we do not publish your email address. It is only used to let you know when your message is published. We do not use it for any other purpose. Please see our privacy policy for more information.
If you write about specific medications or operations, please do not name health care professionals by name.
All opinions are moderated before being included (to stop spam)
Contact Our News Editors
For any corrections of factual information, or to contact the editors please use our feedback form.![]()
Please send any medical news or health news press releases to:
Note: Any medical information published on this website is not intended as a substitute for informed medical advice and you should not take any action before consulting with a health care professional. For more information, please read our terms and conditions.
View the original article here
Eczema Blog
