 We’re told that diamine oxidase’s (DAO) job is to make sure histamine is broken down when it’s no longer needed for things like healing, digestion, and wakefulness. Studies show its activity varies more in women that men, possibly due in part to histamine’s role in causing uterine contractions and miscarriage. While DAO production does decline as we age (especially in women), there are nutrients proven to give it a boost. Read on to find out what they are and how we can get them from whole foods rather than supplements.
We’re told that diamine oxidase’s (DAO) job is to make sure histamine is broken down when it’s no longer needed for things like healing, digestion, and wakefulness. Studies show its activity varies more in women that men, possibly due in part to histamine’s role in causing uterine contractions and miscarriage. While DAO production does decline as we age (especially in women), there are nutrients proven to give it a boost. Read on to find out what they are and how we can get them from whole foods rather than supplements.
Research tells us that DAO is highest during the luteal phase that is right after ovulation and up to menstruation, which is why low serum DAO levels in post menopausal women “should be interpreted with caution”.
While there remains some controversy as to how diamine oxidase is linked to excess histamine, for the purposes of this post I’m just looking at studies speaking of how we can boost this enzyme.
A recent study confirmed what I’ve been writing about for the last few years regarding DAO and nutrients,
and because I’m a fan of getting as many nutrients as possible as food rather than supplements, I created my nutrient and antioxidant dense cookbooks. Check out the books and read about how antioxidants fight histamine inflammation here.
DAO boosting nutrients
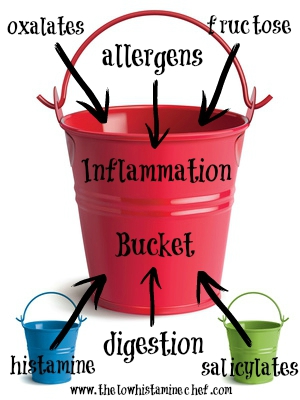
Please bear in mind that some foods are only high histamine because of bacteria contamination or spoilage. Any kind of virus or bacteria will stimulate an inflammatory release of histamine. This is why fermented foods are so problematic for us.
Vitamin B12
Liver (I also suggest grass fed – this appears as high histamine on some lists)
Salmon (fresh gutted fish or flash frozen at sea is not considered high histamine)
Grass fed beef (you can do regular beef but that would be inflammatory, the grass provides the animal with omega 3 fatty acid)
Eggs (duck and chicken, but they can also be inflammatory. I buy flax seed or pastured chicken eggs only)
Chicken (inflammatory so I don’t eat it, pastured may be less so)
Phosphorus
Sunflower seeds (some websites list these as high histamine)
White beans
Mung beans
Grass fed beef
Almonds
Brown rice
Broccoli
Eggs (uncooked egg white is a histamine/mast cell trigger. Ask your doctor if duck eggs might be alright for you)
Long chain/Omega fatty acids
Olive oil is an excellent source of long chain fatty acids. It’s also higher in the monounsaturated fat than vegetable oils, which means it’s less prone to oxidation (we don’t want that which is why we eat antioxidant foods like blueberries).
I eat about a pound of salmon a week for the omega 3 fatty acids. I prefer not to take supplements due to the oxidation of the oil. If you take them, make sure to add in an antioxidant or buy one that comes with it in the capsule.
Calcium
I’ve left out dairy because it’s highly inflammatory and casein is a mast cell trigger
Sesame seeds (listed on some sites as high histamine)
Collared greens
Mustard greens
Beet greens
Broccoli
Chard
Salmon (wild caught is best if possible because farmers sometimes use antibiotics and food dye pellets to colour the salmon)
Sardines (I eat them fresh only, and I mean really fresh because they are rarely gutted)
Zinc
Grass fed meats and poultry (if you can find it)
White beans
Chickpeas
Lentils
Oats
Salmon
White fish
Pistachios
Almonds
Magnesium
Read the histamine magnesium post here.
Chard
Pumpkin seeds
Kefir (fermented foods are considered high histamine)
Black beans
Almonds
Banana (high histamine, never had a problem with them myself but always be careful please)
Cacao (not high histamine but can liberate histamine from mast cells)
Learn how to create your own personalised healing plan here.
It’s finally here! Man Food – a high nutrient antihistamine and anti-inflammatory ingredient filled book geared towards guys, women who love to work out, yoga like they mean it, or just load up on healing nutrients. Features my personal shopping list of antihistamine and anti-inflammatory foods.
The Anti-cookbook and all liquid Anti-Detox Book, don’t treat any conditions, but feature a plethora of the high nutrient antihistamine and anti-inflammatory ingredients that have been instrumental in helping me feed myself on a limited diet. The Anti-cookbook features a four page list of antihistamine and anti-inflammatory foods and comes in regular and Paleo
—REFERENCES—
Miyoshi, Makoto, Manami Ueno, Mari Matsuo, Yasuhiro Hamada, Michiko Takahashi, Masashi Yamamoto, Ikuko Yamamoto, Reiko Mikajiri, Satoko Tabuchi, Kumiko Wakida, Misa Yamanishi, Midori Hirai, and Makoto Usami. “Effect of dietary fatty acid and micronutrient intake/energy ratio on serum diamine oxidase activity in healthy women.” Nutrition 39-40 (2017): 67-70. Web.
“Phosphorus Helps Your Body Detox & Strengthen.” Dr. Axe. N.p., 09 May 2016. Web. 20 June 2017.
Publications, Harvard Health. “The A list of B12 foods.” Harvard Health. N.p., n.d. Web. 20 June 2017.
Calcium. N.p., n.d. Web. 20 June 2017.
“The histamine-(in)fertlity link | Healing Histamine.” Healing Histamine | Histamine Intolerance Diet Foods Recipes. N.p., 11 Dec. 2014. Web. 20 June 2017.
Hamada, Yasuhiro, Yurika Shinohara, Miyuki Yano, Mari Yamamoto, Misa Yoshio, Kumiko Satake, Akiyo Toda, Midori Hirai, and Makoto Usami. “Effect of the menstrual cycle on serum diamine oxidase levels in healthy women.” Clinical Biochemistry 46.1-2 (2013): 99-102. Web.
“Functional Foods Fact Sheet: Omega-3 Fatty Acids.” FoodInsight.org. N.p., n.d. Web. 20 June 2017.


 Conditioned taste aversion is a survival mechanism whereby animals learn to associate taste with a food that has made them sick; usually because it’s toxic or spoiled. In some cases the conditioned association between a food and sickness is so strong that the amygdala, the primitive part of the brain whose role it is to identify whether something is dangerous, can send the danger signal based on just the smell of a food alone. Sound familiar? Read on…references always at the bottom of post.
Conditioned taste aversion is a survival mechanism whereby animals learn to associate taste with a food that has made them sick; usually because it’s toxic or spoiled. In some cases the conditioned association between a food and sickness is so strong that the amygdala, the primitive part of the brain whose role it is to identify whether something is dangerous, can send the danger signal based on just the smell of a food alone. Sound familiar? Read on…references always at the bottom of post. Two important questions regarding fasting for those with histamine intolerance are: does not eating affect the function of the histamine degrading diamine oxidase (DAO) enzyme, and is the stress of not eating so extreme as to negate the benefits of it?
Two important questions regarding fasting for those with histamine intolerance are: does not eating affect the function of the histamine degrading diamine oxidase (DAO) enzyme, and is the stress of not eating so extreme as to negate the benefits of it? 

 A small study has just revealed that scented laundry washes contain carcinogens that may raise cancer risk if inhaled. This is unlikely to be a problem for people with histamine and mast cell disorders given that our heightened sense of smell and reactions to scents, prevent most of us from using them. The question is why do they bother us so?
A small study has just revealed that scented laundry washes contain carcinogens that may raise cancer risk if inhaled. This is unlikely to be a problem for people with histamine and mast cell disorders given that our heightened sense of smell and reactions to scents, prevent most of us from using them. The question is why do they bother us so? Chalk up another one to a dysfunctional immune system – Chronic Fatigue Syndrome (CFS). Researchers recently proved (for the first time), that the condition is not psychosomatic (yeah, thanks for calling us hypochondriacs all these years). This wasn’t news to some: according to NHS funded researcher Dr. Theoharides, CFS is one of many mast cell linked conditions that he has known to be linked for years. It wasn’t so long ago that narcolepsy was pegged to an imbalance of brain histamine levels.
Chalk up another one to a dysfunctional immune system – Chronic Fatigue Syndrome (CFS). Researchers recently proved (for the first time), that the condition is not psychosomatic (yeah, thanks for calling us hypochondriacs all these years). This wasn’t news to some: according to NHS funded researcher Dr. Theoharides, CFS is one of many mast cell linked conditions that he has known to be linked for years. It wasn’t so long ago that narcolepsy was pegged to an imbalance of brain histamine levels.  Have you noticed that your annoying histamine intolerance and mast cell symptoms, particularly fogginess, bloating, headaches and tenderness, get worse just before your period? Yup, it’s your hormones, and the interaction between histamine and estrogen in particular. And now researchers tell us that estrogen is the reason that women have longer anaphylactic episodes than men.
Have you noticed that your annoying histamine intolerance and mast cell symptoms, particularly fogginess, bloating, headaches and tenderness, get worse just before your period? Yup, it’s your hormones, and the interaction between histamine and estrogen in particular. And now researchers tell us that estrogen is the reason that women have longer anaphylactic episodes than men. 
